Due to a recent change in our pharmacy software system, the process for submitting refill requests online has now changed.
Our previous mobile app and your current login credentials will no longer work.
Please click the Refill Button to begin the new process.
Thank you for your patience during this transition.
Note: we do accept walk-in for most routine immunizations including the COVID-19 vaccinations.
Click to make an appointment!
Get Healthy!
- I. Edwards
- Posted April 7, 2025
Biden Plan To Expand Obesity Drug Coverage Is Rejected
The Trump administration has decided not to expand Medicare and Medicaid coverage for popular obesity drugs, blocking a Biden administration initiative that could have helped millions of Americans access the medications.
Catherine Howden, a spokeswoman for the Centers for Medicare and Medicaid Services (CMS), said that expanding coverage for these drugs “is not appropriate at this time,” though it "may consider future policy options” for them.
The decision was included in a 438-page rule updating other parts of Medicare’s drug coverage.
Currently, Medicare covers these drugs only for people with diabetes, or in rare cases, for those who are obese and also have major heart problems or sleep apnea, The New York Times reported.
Former President Joe Biden's plan would have expanded access to people who are obese but do not have other health problems.
Officials estimated that about 3.4 million more people might start using the medications if coverage were expanded.
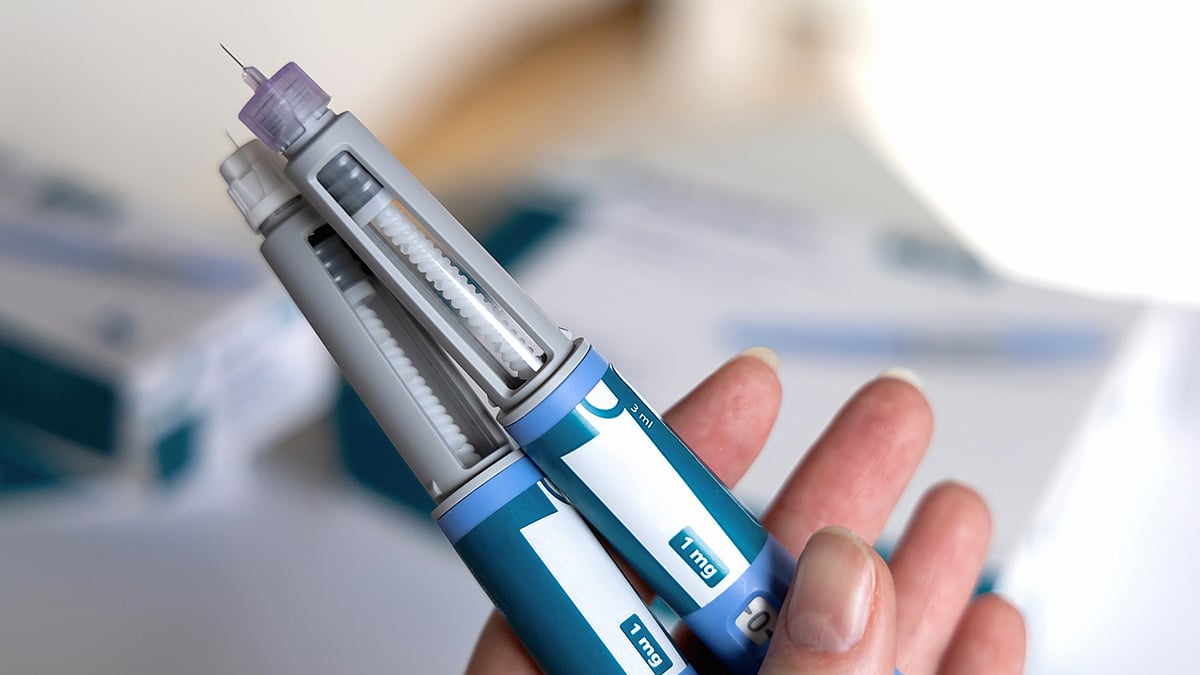
The drugs include Novo Nordisk’s Wegovy and Ozempic, and Eli Lilly’s Zepbound and Mounjaro. These medications have shown benefits beyond weight loss, such as lowering the risk of heart attacks and strokes.
But cost was a major concern. The Congressional Budget Office estimated that expanding coverage would cost the federal government around $35 billion over 10 years, The Times said.
Retail prices for the drugs range from $350 to $500 per month without insurance, according to The Times.
Compounded versions, made during shortages, have cost less than $200 -- but regulators plan to stop allowing those soon.
Some Medicaid programs already cover these drugs. Others don’t.
Proponents argue that the drugs would save money in the long run by preventing costly health issues. However, it’s still unclear whether those savings would actually happen.
Many private health plans also don’t cover these drugs. Some, like state employee plans in North Carolina and West Virginia, dropped coverage after demand and costs soared.
More information
The Social Security Administration has more on the plan for Medicare.
SOURCE: The New York Times, April 4, 2025





